Borsalino Test #20: The war we lost
The war we lost
The most significant challenge of our species
For the past six decades or so political and scientific institutions proved to be completely ill-equipped to deal with cancer. The clamor of this monumental failure will likely reverberate for the decades to come.
It would be great to be able to point out one specific cause of this debacle. The truth is - we all failed collectively. And that happened, sadly, despite all the hard work and extraordinary sacrifice by many frontline workers. So that’s enough of a hunch to suspect the problem runs deeper than we might think.
Mistakes of omissions are significantly worse than errors of commission, and this one is no exception. With my usual knee-jerk negativity, I argue that all our limited knowledge of oncogenes and other cancer catalysts has not translated into significant reductions in mortality. We haven’t done enough.
The secret to battling cancer is to find means to prevent mutations from occurring in susceptible cells or to find means to eliminate those that mutated without compromising normal growth. The conciseness of that statement clearly belies the enormity of the task.
That’s why scientifically cancer remains a black box. A mysterious entity that was best cut away en bloc rather than treated by some deeper medical insight. To cure cancer (if it could be cured at all), we adopted only two strategies: excising the tumor surgically or incinerating it with radiation. Either the hot ray or the cold knife.
Physicians performed root-and-branch treatments in an effort to exterminate every last vestige of cancer. They would cut more and more tissue from patients’ bodies and administer higher and higher doses of chemotherapy and radiation. They adhered to a kind of bravado that looks a lot like the Hippocratic oath upside down.
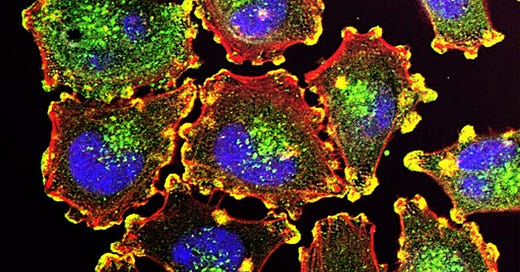
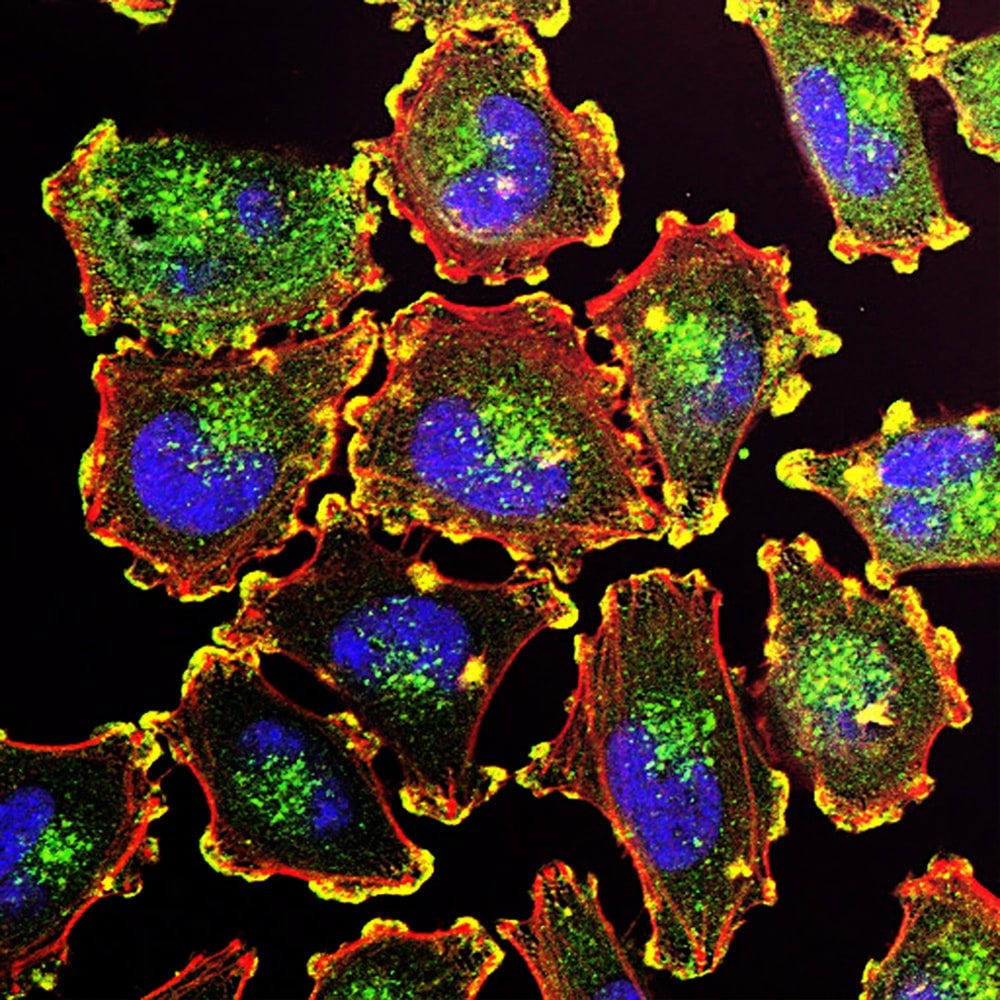
But cancer is built into our genomes. The genes that unmoor normal cell division are not foreign to our bodies, but rather mutated, distorted versions of the very genes that perform vital cellular functions. And cancer is imprinted in our society too. As we extend our life span as a species, we inevitably unleash further malignant growth. If we seek immortality, then so, too, in a rather perverse sense, does the cancer cell.
Malignant growth and normal growth are so genetically intertwined that unbraiding the two might be one of the most significant scientific challenges faced by our species.
No silver bullet
You can appreciate the magnitude of our failure in the numbers. In 1971, President Richard Nixon declared war on cancer, vowing that the disease would be cured within five years. Since then, the National Cancer Institute has spent way over $100B on research.
Skeptics warned that declarations of imminent victory were grossly premature, and they turned out to be right. The overall death rate for cancer has fallen by only 5 percent since 1950. Five! During this same period, the death rate for heart disease plummeted 64 percent and for flu and pneumonia 58 percent.
The decline in cancer mortality since 1950 has not been steady. The rate actually increased from 1950 through the early 1990s and then began dropping. The mortality rate actually rose for two decades after Nixon declared war before dipping downward.
The much-touted drops in cancer rates were mostly attributable to scientific breakthroughs and a decline in smoking. The linkage of cancer to tobacco smoking was a triumph of epidemiology that has been hard to replicate. It is extraordinarily difficult to trace cancer clusters to specific environmental factors.
Cancer-research boosters often state that people are surviving cancer for longer periods. But that is because men and women are being screened more frequently with higher-resolution tests and hence being diagnosed with cancer at earlier stages. They are living longer after diagnosis, not living longer in absolute terms.
This is not a failing of the existing screening approaches as much as it is a product of the fact that most cancers that eventually claim people’s lives are ones we do not screen for, and they are only detected when signs or symptoms are present, usually signifying advanced disease.
The current mortality rate for all cancers in the US is roughly what it was in 1930. Although the death rates of some cancers, notably of the stomach and breast, have recently declined, death rates of liver, pancreatic, and brain cancer have increased. Absolute death tolls from cancer keep climbing in the US, increasing from less than 300,000 victims in 1990 to over 600,000 in 2020.
The more we learn about cancer’s hideously complex, shape-shifting etiology, the less likely it seems that we will vanquish it once and for all. Knowledge of cancer’s biology is unlikely to eradicate cancer from our lives. No simple, universal, or definitive cure is in sight. And is never likely to be. We must accept this fact and yet keep fighting, avoiding the extremes of delusional hope and defeatism.
How to control a public health crisis
Cancer is a progressive disease. Virtually all solid tumors develop as benign lesions that progress at an arbitrary rate, culminating in metastatic diseases. As cancer evolves, the number of treatment options shrinks. The survival rate for a person diagnosed with cancer once it has already spread is just 21%, compared to 89% of someone whose cancer is found in the early stages. Hence the importance of early screening.
Science begins with counting. The various single cancer screening tests, combined with their respective rates of compliance and test performance, results in approximately 15% of the 1.3 million cancers diagnosed each year, being detected early among those aged 50-79. And finding those cancers is inefficient, with $25 billion spent annually to identify approximately 200,000 cancers while spinning off nearly 9M false-positive results.
If we view cancer morbidity and mortality as a public health problem rather than a clinical one, we can operate a major paradigm-shift. In that respect, our problem is not unlike that of population management during Covid. We widely agreed that we need to dramatically increase Covid testing and detection to get control of this public health crisis.
Similarly, we would need to open the aperture from just looking at cancer test characteristics - like false positive rate - and begin to look at infection detection rates in the population. It is well recognized that improving early cancer detection may be the only way to really put a dent in the cancer mortality curve.
So, what if we developed a different approach? What if we could transition from screening for individual cancers and start screening individuals for all their cancers? What if we dramatically improved overall cancer detection? What if we tracked the Cancer Detection Rate (CDR) in the population?
Cancer Detection Rate (CDR) is the number of cancers detected divided by the number of cancers expected in the population monitored. This could be applied to health systems, metropolitan statistical areas, states, and countries. So, it is a population sensitivity measure normalized for cancer incidence.
Using the US as an example, if the population is 107 million Americans between age 50-79, the CDR for mammography would be 9%, because it detects approximately 117,000 cancers of the 1.3 million expected. Similarly, with stool-based colorectal cancer screening, the CDR is about 6% (69,000 detected). So, even when all five single cancer screening tests are combined, the CDR is approximately 16% (206,000 detected). While an enormous accomplishment, this alone will not bend the cancer mortality curve or address cancer's public health crisis.
With the genomic revolution and advances in machine learning, there are now several multi-cancer early detection (MCED) tests near commercial use, and the CDR may be the right way to assess our progress.
It is estimated that If everyone took an annual MCED blood test that detects multiple cancers in addition to current screening measures, it could produce a CDR of 50% for all cancers and 75% for the deadliest cancers (e.g. those with 5-year survival less than 50%).
Why is MCED such a profound idea? Because developing and testing a new screening approach for each cancer, then building capacity to manage the downstream complications and false positives, is just unworkable.
So, these tests may miss some cancers, thus they must be used in addition to existing single cancer screening. But today, there is no approach to early detection of most cancer killers, and so, from a population health perspective, even a 50% average sensitivity across cancers could lead to the discovery of many cancers before their clinical diagnosis, and potentially at earlier stages where treatments are more effective and potentially curable.
The advent of technological innovation provides an opportunity for us to evolve our approach. But we need to learn the lessons from decades of cancer research and the public health challenges posed by COVID-19. Just as we track COVID-19 infection rates, detection rates, and death rates by city, state, and nation, we need to embrace CDR and track our progress in early cancer detection.